Merkel cell carcinoma, the disease that killed Jimmy Buffett: What to know about this illness
Music icon Jimmy Buffett passed away on Friday at the age of 76.
The cause of death was merkel cell carcinoma (MCC), a disease he had been fighting for four years, according to the official obituary posted on the musician’s website.
MCC is a rare but aggressive type of skin cancer that is known to have a high rate of recurring and spreading, according to the Skin Cancer Foundation (SCF).
LEGENDARY MUSICIAN JIMMY BUFFETT DEAD AT 76: ‘LIVED HIS LIFE LIKE A SONG TIL THE VERY LAST BREATH’
Around 3,000 cases are diagnosed in the U.S. each year.
That number is expected to reach 3,250 by 2025.
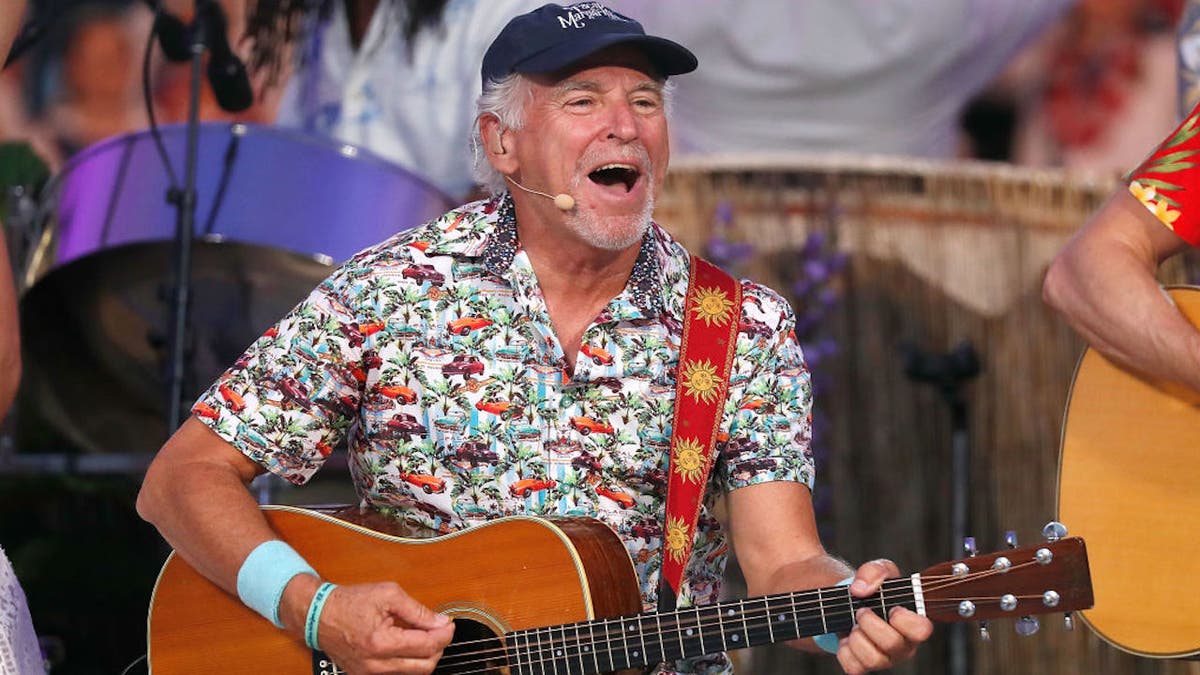
Music icon Jimmy Buffett passed away on Friday at age 76. The cause of death was merkel cell carcinoma (MCC), a disease he had been fighting for four years. The illness is 40 times more rare than melanoma. (Getty Images)
The disease is 40 times rarer than melanoma, the SCF states on its website.
Who is at risk?
The primary cause of Merkel cell carcinoma is “excessive exposure to natural or artificial sunlight,” according to the Mayo Clinic.
Certain groups of people are at a higher risk, however.
Those whose immune systems have been weakened by a medical condition or certain immunosuppressant medications may be more susceptible to the disease, per the SCF.
MUSIC ICON JIMMY BUFFETT’S CAUSE OF DEATH REVEALED
Compared to those with healthy immune systems, immunocompromised people are 15 times more likely to develop MCC.
A history of other types of skin cancers — including melanoma, squamous cell carcinoma and basal cell carcinoma — is another risk factor.
Around 3,000 cases of MCC are diagnosed in the U.S. each year, and that number is expected to reach 3,250 by 2025. (iStock)
Most people who are diagnosed with MCC are males and are over 50 years old, the SCF stated.
Fair-skinned people also have a higher risk of developing the disease.
What should people look for?
The most common symptom of MCC is a shiny or pearly lesion or nodule found on the skin — usually in areas that are frequently exposed to the sun, per the SCF.

Merkel’s tumor of the shoulder is shown here in a 61-year-old man. (Getty Images)
These painless growths are usually around 1.7 centimeters in size — about the size of a dime — at the time of detection.
The lesions are skin-colored, red, purple or bluish-red, according to the SCF.
They tend to expand quickly.
What are the challenges of diagnosis?
Early detection is key to the successful treatment of Merkel cell carcinoma, but this type of skin cancer can prove to be more challenging to diagnose.
Studies have shown that 56% of Merkel cell carcinomas were mistaken for benign cysts or infected hair follicles when first examined by doctors, the SCF stated.
BE WELL: CATCH SKIN CANCER WARNING SIGNS EARLY WITH REGULAR SELF-EXAMS
Some cases also originate in areas where they are difficult to detect — including the mouth, throat and nasal cavity.
The foundation also pointed to a study that found 14% of MCCs had already spread to the lymph nodes without the appearance of a tumor.

Those who notice any unexplained changes in the skin should contact a dermatologist for a skin check. (iStock)
Dr. Michael Whitlow, a dermatologist at NYU Langone Health, reiterated that Merkel cell carcinoma can look somewhat nondescript and is often missed.
“I have seen one case in my years of practice,” he told Dr. Marc Siegel, a Fox News contributor. “It was on the cheek, and when I saw it, I initially thought it was just an unusual angioma.”
He added, “In general, it is fairly aggressive — even with people who have localized disease.”
“It can kill you in as fast as three weeks, especially when it’s on the head and neck.”
Dr. Doris Day, another dermatologist at NYU Langone Health, called MCC “the deadliest of all the skin cancers.”
As she told Siegel, “It’s the one I fear the most and am always on the lookout for.”
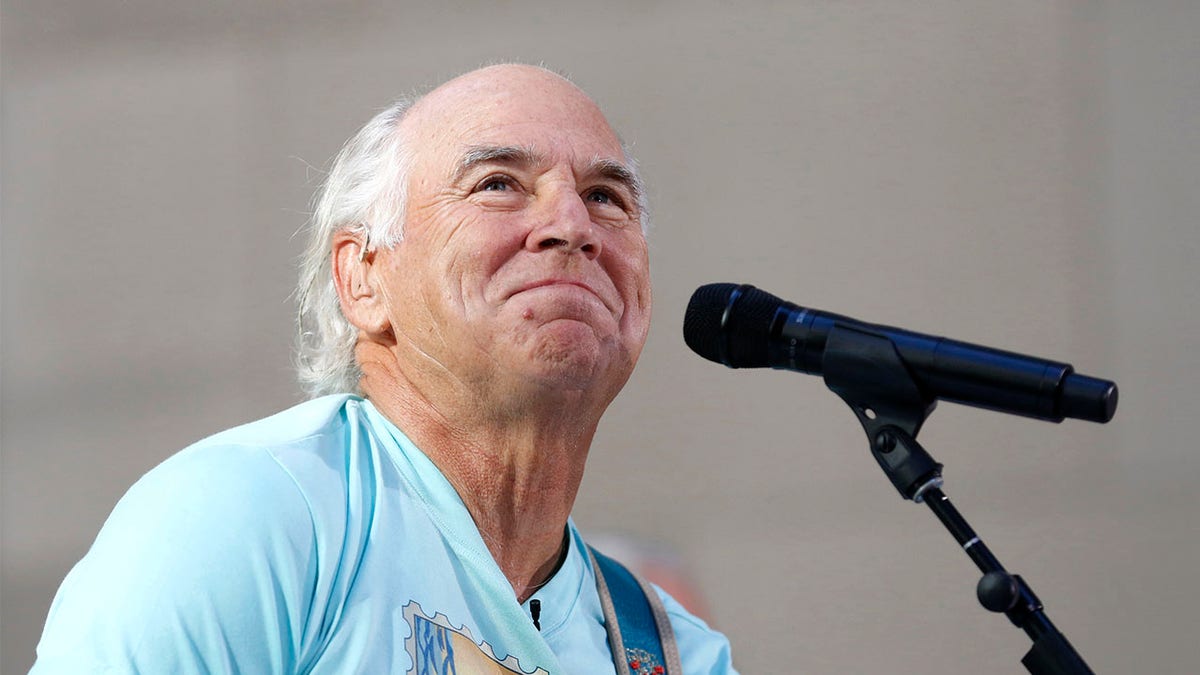
Singer Jimmy Buffett is shown performing on NBC’s “Today” show in New York City, Aug. 15, 2013. The musician passed away on Friday, Sept. 1, from Merkel cell carcinoma. (REUTERS/Brendan McDermid)
“It can kill you in as fast as three weeks, especially when it’s on the head and neck,” she added.
Day also pointed out the cancer’s relatively non-specific appearance, which can mean it’s misdiagnosed as an inflamed cyst or benign skin nodule.
What is the viral connection?
Recently, Day noted, researchers have made a connection to a virus that can trigger Merkel cell carcinomas.
Studies have shown that a virus called Merkel cell polyomavirus (MCPyV) is associated with about 80% of MCC cases.
SKIN CANCER CHECKS AND SUNSCREEN: WHY THESE (STILL) MATTER VERY MUCH FOR GOOD HEALTH
MCPyV is the only polyomavirus that has been found to be linked to human cancer, according to the Center for Emerging and Re-emerging Infectious Diseases (CERID).
The virus is very common, but most healthy adults don’t experience any symptoms.
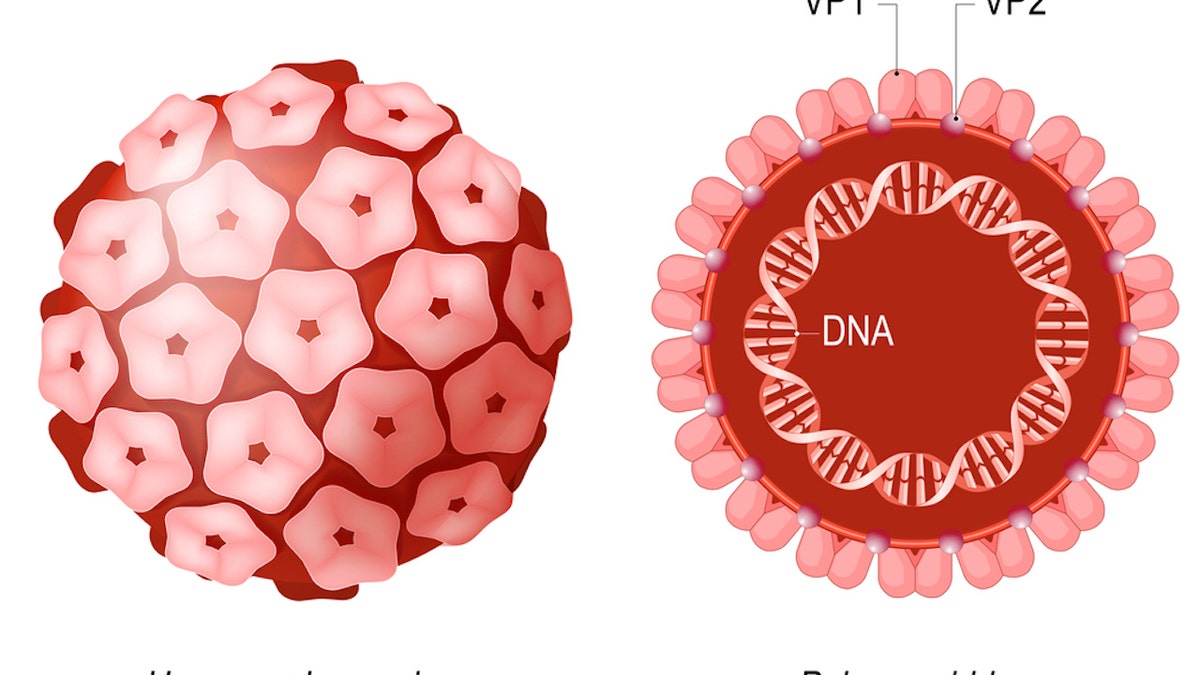
Studies have shown that a virus called Merkel cell polyomavirus (MCPyV) is associated with about 80% of MCC cases. (iStock)
Older people and those with weakened immune systems are more likely to develop MCC as a result of the virus, CERID states on its website.
What are the treatment and prognosis?
After a diagnosis of MCC — via a physical exam, skin exam and skin biopsy — fast treatment is critical to extending survival.
Prognosis and treatment are based on the stage of the cancer, its location on the body, the patient’s age and health, and whether it’s a first-time cancer or a recurrence, according to the National Cancer Institute.
MORE YOUNGER PEOPLE ARE RECEIVING CANCER DIAGNOSES, STUDY FINDS — ESPECIALLY THIS TYPE
The standard treatments for MCC include surgery, chemotherapy, radiation therapy and immunotherapy.
Due to the viral nature of many MCC cases, “some of the latest treatments for widespread disease are immunotherapy-based,” Dr. Marc Siegel, clinical professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, told Fox News Digital this weekend.

Applying sunscreen before sun exposure is one of the primary methods of preventing Merkel cell carcinoma. (iStock)
With immunotherapy, the treatment boosts the patient’s immune system so it is better equipped to fight cancer.
Additional treatments are being tested in clinical trials.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
For patients with localized Merkel cell carcinoma that has not spread, the five-year survival rate is 75%, according to the American Cancer Society.

The standard treatments for MCC include surgery, chemotherapy, radiation therapy and immunotherapy. (iStock)
For those whose cancer has started to spread to nearby areas or lymph nodes, the survival rate is 61%.
Five-year survival drops to 24% for patients whose cancer has spread to more distant parts of the body, the ACS states.
What are some prevention tips?
As with other skin cancers, wearing sunscreen with an SPF of 60 or greater is recommended to prevent the development of Merkel cell carcinoma, according to Cleveland Clinic.
CLICK HERE TO GET THE FOX NEWS APP
Experts also advise avoiding direct contact with the sun between the hours of 10 a.m. and 4 p.m., and to avoid using tanning beds or sunlamps.
When in direct sunlight, it’s wise to cover the skin as much as possible and/or wear a wide-brimmed hat and large sunglasses, per Cleveland Clinic.
Doctors recommend performing regular skin checks at home and contacting a health care provider if any unexplained changes are found.
